Billing is one of the most error-prone and time-consuming parts of running a healthcare practice. Manual coding, data entry, and claims submission slow down reimbursements and increase the likelihood of denials. Automated superbill generation removes these friction points by creating accurate, itemized statements that simplify coding, improve patient understanding, and speed up your insurance claims process. When practices reduce manual work clients get reimbursed faster. This creates a smoother billing experience for everyone involved.
Key Takeaways
- Superbills are itemized, detailed lists of services rendered to a patient.
- Manual billing practices create many challenges, including coding errors, slow processing times, lags in cash flow, and heavy administrative workloads.
- With superbills, staff can create these for clients' reimbursement for services rendered and paid, creating a positive impact on cash flow and the patient experience.
If there’s just one area in healthcare operations that could benefit from automation, it’s the billing process. Healthcare billing is a complex process largely driven by manual efforts, which slows down insurance claims management and reimbursements. Because 1 in 10 claims are denied, it’s important to get the details right the first time. This process will help clients avoid unnecessary denials as well.
Medical billing requires a team of billing specialists who match services with insurance codes, manually enter details, reconcile statements, and interact with customers, healthcare providers, and insurance companies — for every patient served.
Automated superbill generation can simplify and speed up the process, making it easier for clients and insurance companies. Here’s how better billing practices can have a positive impact on finances, operations, and patient satisfaction.
What Is a Superbill?
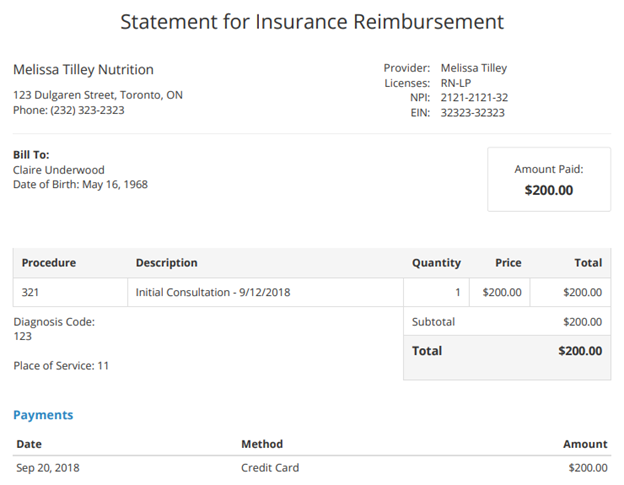
A superbill is an itemized document listing diagnoses, procedures, provider details, and relevant patient information. Both patients and insurance companies use superbills to understand what services were provided and how they should be billed. Automated superbills ensure that every code and charge is clear, accurate, and ready for submission.
This feature is usually part of a complete healthcare billing software package.
Practices use automated billing solutions to serve as a bridge between patient care and insurance reimbursement. They reduce the number of questions about billing, and they give clients an easier way to request reimbursements from insurance companies.
Why Manual Medical Billing Leads to Errors and Delays
Manual billing processes slow down your claims cycle and create avoidable administrative work. Common issues include:
- Coding errors. Insurance billing involves complex medical codes that, when entered incorrectly, can lead to denials or delays. Assigning incorrect or outdated codes, collecting inaccurate patient information, and using manual claims submissions instead of automation are the top challenges facing medical billing.
- Slow processing times. Manual workflows can slow down billing, with each step requiring time and human oversight.
- Administrative overload. Manually handling billing requires significant time and staff, especially when you run into coding errors and claims corrections.
Automated superbills solve these challenges. With automated billing, the coding process is done for you to minimize time, reduce billing errors, ease the admin workload, and improve timely payments.
How Automated Superbill Generation Streamlines the Claims Process
Automated superbill generation improves billing accuracy and eliminates repetitive tasks.
One of its superpowers lies in its itemization structure. Superbills structure each item line by line, code by code, so that patients and insurance companies can easily understand what’s being billed. This supports a more efficient process while reducing errors and fostering patient trust and satisfaction. Key benefits include:
- Accurate, Standardized Coding. Automated superbills apply correct codes consistently, reducing the risk of denials or rejected claims.
- Clear, Itemized Documentation. Line-by-line itemization helps patients and insurance companies understand the charges, supporting a smoother claims review.
- Support for Price Transparency Requirements. Detailed superbills help practices meet federal expectations for clear, accessible billing information.
Superbills also support recent laws regarding pricing transparency and accessibility that hospitals now have to provide.
With automatically generated superbills, client can submit them immediately to insurance companies, accelerating the claims submission process. What used to take potentially hours per patient can now be done in seconds.
Billing staff can free up time spent on coding.
Financial Impact: Faster Reimbursements and Stronger Cash Flow
When claims are accurate on the first submission, practices avoid costly delays and patient disputes. Automation frees staff to process more in less time, reducing overhead and improving the consistency of incoming revenue.
Faster billing reduces the time between service delivery and payment, allowing practices to get paid faster and with fewer errors. With timely payments, there’s a constant, reliable cash flow so practices can pay their own bills on time and continue providing a high level of patient care.
By automating the superbill process, practices can reduce the time and costs associated with billing. Billing staff can process more and bill in less time, freeing up time to handle disputes, conduct follow-ups, and keep cash coming in.
How Superbills Improve Patient Transparency and Trust
Patients want clear, understandable healthcare costs. Automated superbills:
- Show exactly what services were provided
- Reduce confusion and billing inquiries
- Help patients understand and settle balances sooner
Transparent billing supports patient satisfaction and strengthens trust in your practice.
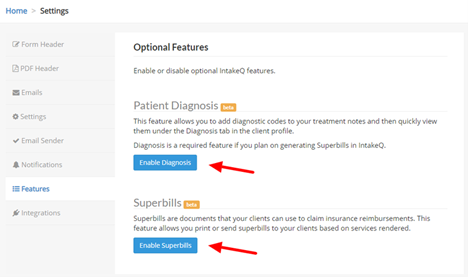
Using PracticeQ Superbill Automation in Your Billing Workflow
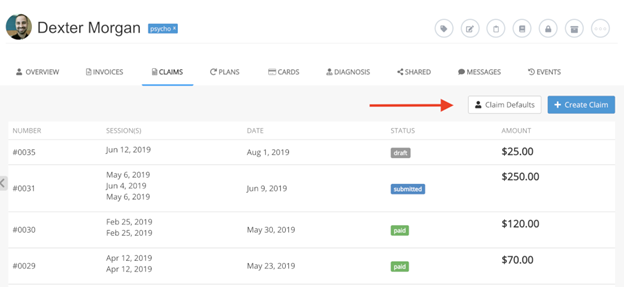
PracticeQ simplifies every stage of the billing process—from coding to submission—so practices can reduce errors, improve reimbursement speed, and maintain a healthier financial foundation. With automated superbills, your team can focus on supporting patients instead of fixing billing mistakes.
Explore PracticeQ superbill automation by scheduling a demo or starting a free trial.
Superbill FAQs
What is a superbill in medical billing?
A superbill is a detailed, itemized document listing diagnoses, procedures, and provider information. It serves as the primary source for insurance claim submissions and helps patients understand their charges.
How does automated superbill generation reduce claim denials?
Automation applies accurate, up-to-date codes and eliminates manual entry errors, which are among the most common reasons claims are rejected by insurers.
Why is manual billing so time-consuming for healthcare practices?
Manual billing requires staff to review codes, enter data, correct errors, respond to payer requests, and reconcile statements—tasks that automation can complete in seconds.
How do superbills support patient transparency requirements?
Superbills clearly itemize services and costs so patients understand their charges, supporting compliance with federal price transparency regulations and reducing billing disputes.
What financial benefits can practices expect from automated superbills?
Practices gain faster reimbursements, fewer denials, reduced administrative workload, and a more predictable cash flow.
FAQs
Healthcare claim denial statistics: State of Claims Report 2024. (2024, October 4). Experian.
Challenges of Medical Billing and Coding. (2023, June 2). Avila University.
Hospital Price Transparency. (2024, September 10). Centers for Medicare & Medicaid Services.
https://www.cms.gov/priorities/key-initiatives/hospital-price-transparency


