How Practices Are Resetting Operations for the Year Ahead
Key Takeaways
- Practice efficiency is the defining healthcare trend for 2026 as rising costs and staffing constraints leave little room for wasted time.
- The biggest efficiency gains come from tightening everyday workflows, not adding more tools or staff.
- AI delivers the most value when it’s embedded into operations, supporting documentation, intake, scheduling, and administrative work without replacing clinical judgment.
- Scheduling, digital intake, self-service, and integrated payments now play a central role in protecting capacity and reducing staff burden.
- PracticeQ gives practices one system to run the day more efficiently, without added complexity.
As healthcare trends continue to reshape how practices operate in 2026, one reality is clear: running a practice is more expensive, more complex, and less forgiving than it used to be.
For your practice, staying ahead now means being deliberate about how work flows through the day, so pressure doesn’t turn into chaos. Below, we break down the practice efficiency trends shaping 2026 and where AI is delivering the clarity and control practices need to operate with confidence.
Why Practice Efficiency Is the Defining Healthcare Trend for 2026
In 2026, small inefficiencies have bigger consequences.
Last year, 90% of medical practices reported higher year-over-year operating costs, largely driven by staffing expenses and persistent workforce shortages. When it costs more to staff your practice and harder to add capacity, there’s less room to absorb wasted time.
As a result, efficiency is a defining healthcare trend in 2026 because it’s one of the few levers still fully within your control. Between tighter workflows, fewer handoffs, and AI-powered technology, you can take back control over how the day runs.
Here’s what practices are prioritizing next:
Trend 1: AI Moves from “Nice to Have” to Built-in Workflow Support
AI in healthcare is no longer judged on potential. It’s judged on whether it fits into the way your day actually works.
With full schedules and little room for rework, new tools earn their place only if they reduce effort without creating cleanup later. The AI tools that last operate inside existing workflows, take work off the plate without shifting it elsewhere, and support the day instead of reshaping it.
AI Notes Reduce After-hours Charting
With AI-assisted documentation, charting stays closer to the visit itself. Notes are drafted while context is fresh, allowing you to review and complete documentation sooner instead of reopening it later.
That shift gives you more control over when charting happens. Rather than letting documentation spill into personal time, you can contain it to the window where it belongs.
AI Supports Accuracy, Not Autonomy
Practices aren’t using AI to make decisions. They’re using it to reduce effort.
AI supports drafting, organizing, and maintaining momentum, while clinicians remain accountable for every final call. Used this way, AI doesn’t replace expertise. It protects it.
Trend 2: Scheduling Becomes a Capacity Management Tool
Scheduling is one of the clearest ways to protect capacity without adding staff.
When scheduling is treated as a static calendar, inefficiency doesn’t disappear. It shifts into uneven days, staff strain, and growing administrative work. Practices that run more predictably treat scheduling as an operational decision, paying attention to how time is used and how much pressure the day can realistically absorb.
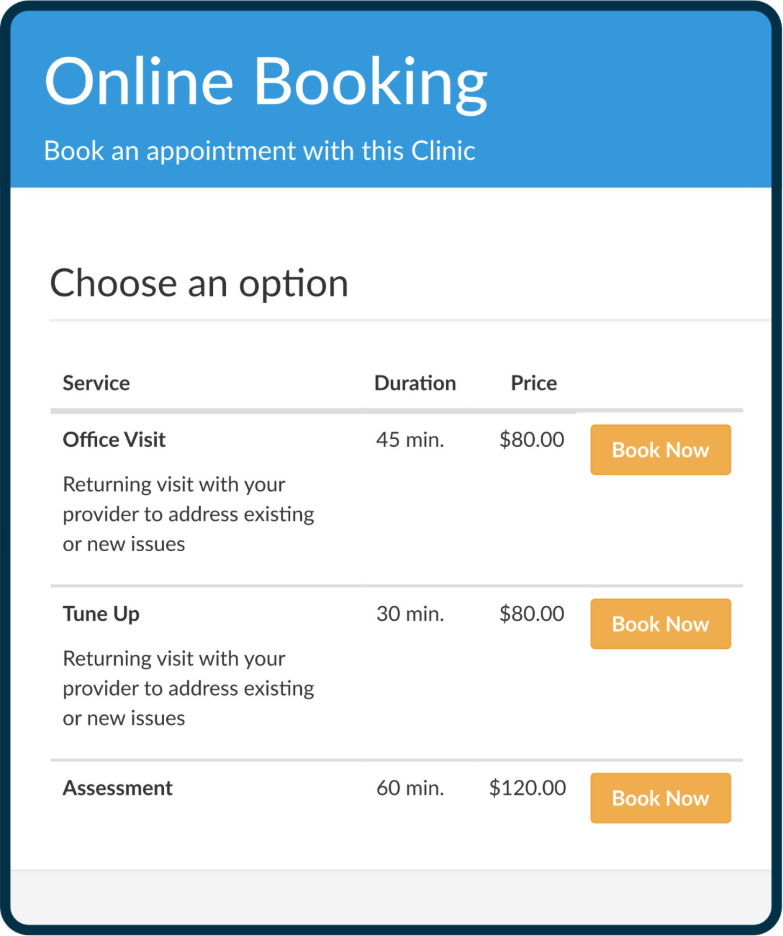
Automated Booking Reduces Front-desk Load
Online booking helps when it removes routine work without creating more of it later. Clear rules and guardrails prevent follow-up calls, clarifications, and manual fixes from landing back on the front desk.
As a result, staff spend less time managing availability and more time supporting patients and coordination that require human judgment.
Trend 3: Digital Intake Replaces Manual Data Handling
Manual intake has become a visible source of inefficiency. What once felt like a front-desk issue now affects visit flow, documentation, and billing.
Handled manually, intake leads to missing forms, repeated questions, and providers starting visits without full context. Practices are responding by moving intake earlier, preparing visits in advance instead of assembling them at check-in.
Digital intake tools collect information before the visit, flag incomplete fields, and route accurate data directly into clinical and administrative workflows.
Forms Become Pre-Visit Gatekeepers
When demographics, insurance, medical history, and consent are completed ahead of time, appointments arrive ready. Missing information is resolved before arrival, reducing interruptions and keeping schedules on track.
Cleaner Data Improves Downstream Efficiency
By having complete intake data, you have less work to deal with down the line. You get more accurate documentation, fewer billing issues, and timely follow-up that doesn’t stall over missing or inconsistent information.
Trend 4: Patient Self-Service Becomes the Default Expectation
Patient self-service now defines how many patients expect to interact with your practice. In fact, more than half of U.S. adults use a patient portal when their provider offers one, signaling that self-service tools are already part of everyday healthcare behavior.
At that level of adoption, self-service removes work from staff workflows. Tasks that still require staff involvement pull time away from keeping visits on schedule and care coordinated, which is why self-service now shows up as an efficiency driver, not just a patient experience feature.
Trend 5: Revenue Workflows Tighten as Margins Shrink
As margins shrink, revenue workflows are becoming just as critical as clinical operations. You don’t just need to get paid. You need to get paid on time and without creating unnecessary follow-up work.
If your revenue process relies on manual follow-up, disconnected systems, or delayed handoffs, the cost can show up quickly. These conditions extend payment timelines, increase reconciliation work, and reduce visibility into cash flow.
That’s why practices are paying closer attention to how revenue moves through the day, not just what gets billed.
Integrated Payments Reduce Billing Friction
Integrated payments help when they remove steps instead of shifting them. When invoicing, collection, and posting live inside the same workflow, much of the back-and-forth disappears.
As a result, automated charges tied to visit completion reduce follow-up calls, reminder emails, and reconciliation work, allowing teams to focus on exceptions that need attention.
Faster Payments Improve Cash Flow Visibility
Late or inconsistent payments make budgeting harder, delay hiring decisions, and create uncertainty because it’s harder to see what’s been billed, paid, and still outstanding. Streamlined revenue workflows restore that visibility in real time, reducing follow-up work and making cash flow more predictable.
Trend 6: Prescribing, Labs, and Inventory Move into Everyday Efficiency Work
Prescription refills, lab follow-ups, and supply tracking rarely feel like the biggest problems in a practice. But across a full day, they generate a steady stream of interruptions that break focus, slow visits, and pull staff away from patient care.
This is where efficiency work often moves next. Not because these workflows are complex, but because they touch so many moments in the day.
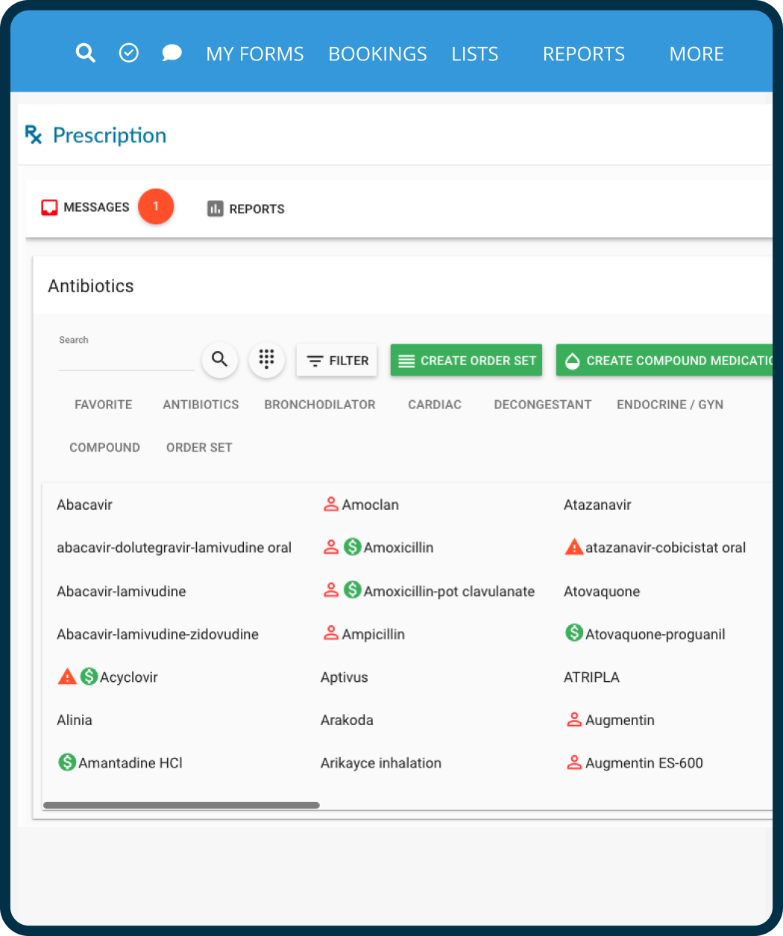
e-Prescribing Reduces Callbacks and Refill Churn
Refill requests and pharmacy questions often surface at the worst possible moments. When they live outside your main system, even simple actions require extra steps and follow-up. Integrated e-Prescribing keeps prescriptions, refills, and insurance context together, so routine requests are resolved quickly without forcing providers to switch systems or interrupt care.
Inventory and Lab Workflows Reduce Manual Oversight
Inventory usage and lab coordination depend on steady tracking, but manual checks tend to slip on busy days. Keeping these workflows tied to the patient record provides a consistent view of usage, reorders, and outstanding results, reducing delays without relying on memory or repeated follow-up.
Trend 7: Consolidation Beats Tool Sprawl
Managing too many systems slows a practice down. Between multiple logins, overlapping features, and disconnected data, routine work requires constant context switching and piecing together information that should already live in one place.
Integrations Reduce Context Switching
Every additional system creates another place to check and another workflow to manage. Staff re-enter information and lose focus just to complete routine tasks.
Integrations keep workflows connected so scheduling, documentation, billing, communication, and reporting move together instead of competing for attention.
Unified Platforms Improve Operational Visibility
When data is spread across systems, it’s harder to understand how the practice is performing. Reporting takes longer and decisions rely on partial information.
A unified platform provides a clearer, more immediate view of operations, making it easier to track performance and adjust without reconciling multiple tools.
Consolidation isn’t about cutting software for the sake of it. It’s about reducing friction and making the systems you rely on easier to run day to day.
Ready to take control of practice efficiency in 2026?
Explore how PracticeQ supports more efficient workflows across scheduling, intake, payments, and documentation.
FAQs
How is AI actually used in healthcare operations today?
Will artificial intelligence replace staff in medical practices?
What healthcare trends matter most for practices in 2026?
How do efficiency trends affect patient experience?
Do practices need new technology to prepare for 2026?
Addressing Health Care Workforce Shortages. (2025, July 16). NIHCM Foundation. https://nihcm.org/publications/addressing-health-care-workforce-shortages
Harrop, C. (2025, June 11). Medical practice operating costs are still rising in 2025 — here’s how to control them. Medical Group Management Association (MGMA). https://www.mgma.com/mgma-stat/medical-practice-operating-costs-are-still-rising-in-2025-heres-how-to-control-them
McCarthy, D. (2025, July 23). Improve Patient Collections Without Hurting Satisfaction. PracticeQ. https://www.practiceq.com/resources/how-to-improve-patient-collections-without-hurting-satisfaction
Norton, C. (2025). HIPAA-Compliant Digital Forms: Why Your Practice Needs Them. PracticeQ. https://www.practiceq.com/resources/hipaa-compliant-digital-forms
Sezgin, E. (2023). Artificial intelligence in healthcare: Complementing, not replacing, doctors and healthcare providers. Digital Health, 9(PMC10328041). https://doi.org/10.1177/20552076231186520
Strawley, C., & Richwine, C. (2023, October). Individuals’ access and use of patient portals and smartphone health apps, 2022. HealthIT.gov. https://www.healthit.gov/data/data-briefs/individuals-access-and-use-patient-portals-and-smartphone-health-apps-2022


