Are You Losing Revenue? 5 Medical Billing Mistakes You Need to Fix
Many healthcare practices are unknowingly losing thousands each year due to avoidable billing errors.
Denied claims, delayed payments, and frustrated patients are more than just admin issues—they’re revenue leaks that hurt your bottom line. But the good news? You can fix them.
We’re breaking down the five most common medical billing mistakes and how to correct them to improve cash flow, reduce administrative burden, and enhance patient satisfaction.
1. Failing to Verify Patient Insurance Before the Visit
Insurance verification is the foundation of clean claims—and revenue protection. Too often, busy front desk teams skip this step or rely on outdated information, which puts reimbursement at risk before the appointment even begins.
Why It Happens
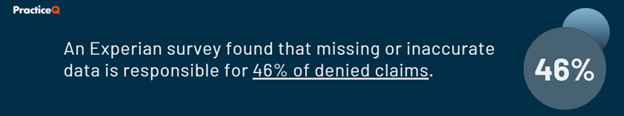
Many claims are denied simply because patient insurance details weren’t updated before the appointment. Coverage changes, incorrect eligibility status, and misclassified provider networks are all common culprits.
How to Fix It
- Verify in real-time. Always check eligibility right before appointments to catch any last-minute changes.
- Automate insurance verification. Integrate it with your billing system or clearinghouse to eliminate manual errors.
- Train staff to verify proactively. Build checks into your intake workflow so coverage status isn’t missed.
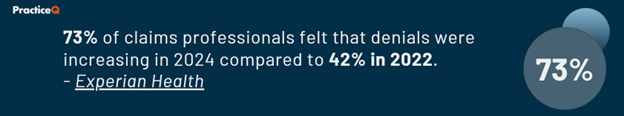
2. Incorrect or Incomplete Medical Coding
Accurate coding is the linchpin of proper reimbursement. Coding errors don’t just lead to payment delays—they can also result in compliance risks, audits, and lost trust with both payers and patients.
Common Mistakes
- Upcoding: Billing for a higher service level than provided.
- Undercoding: Failing to bill for all services delivered.
- Outdated codes: Using old or incorrect ICD-10, CPT, or HCPCS codes.
How to Fix It
- Train and retrain your billing team. Ongoing education on coding updates is non-negotiable.
- Use built-in coding assistance. Choose systems that flag incorrect or missing codes.
- Audit regularly. Catch small issues before they become large revenue drains.
3. Not Submitting Claims on Time
Even perfectly coded claims won't be paid if they’re submitted late. Filing windows are often non-negotiable for payers, and once they close, practices lose that revenue permanently.
Why It Happens
- Late submissions due to overwhelmed admin teams
- Missing documentation
- Failure to track or resubmit denied claims
How to Fix It
- Track deadlines. Use a claims tracking tool to monitor submission windows.
- Automate submissions. Reduce bottlenecks by sending claims directly from your EHR.
- Follow up consistently. Set reminders for claim denials and pending payments.
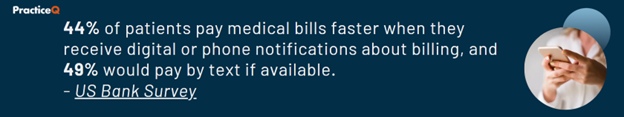
4. Ignoring Patient Balances and Collections
Patient payments now make up a growing portion of practice revenue—but collections often fall through the cracks. If your practice isn't actively managing balances, you're leaving money on the table.
Where Practices Go Wrong
- No cost transparency before treatment
- Late or no payment reminders
- Limited or outdated payment options
How to Fix It
- Provide estimates upfront. Patients appreciate clarity.
- Automate reminders. Send SMS and email nudges about outstanding balances.
- Offer flexible payments. Monthly plans and digital options increase collection rates.
5. Not Analyzing Billing Reports and KPI
You can’t fix what you don’t measure. Reporting helps you move from reactive to proactive revenue cycle management.
Why This Matters
Without regular performance tracking, your billing processes operate in the dark. You miss:
- Denial trends
- Inefficiencies in workflows
- A/R that’s aging out
How to Fix It
- Review analytics regularly. Monthly reviews of denial rates, collection rates, and claim cycles help spot issues early.
- Use a dashboard. Monitor key revenue cycle metrics in real time.
- Optimize based on data. Adjust workflows based on patterns—not assumptions.

How PracticeQ Helps You Eliminate Medical Billing Mistakes
Avoiding billing mistakes takes more than checklists—it takes smart, integrated technology. PracticeQ provides a full suite of revenue cycle tools built to help you:
- Automate insurance verification so you catch coverage issues before they cause problems.
- Validate coding accuracy using built-in tools that flag errors before submission.
- Submit and track claims with automation that ensures deadlines are met and denials are reworked.
- Engage patients in payments with digital billing, payment plans, and automated reminders.
- Get actionable analytics with billing reports and KPI dashboards to fine-tune performance.
With PracticeQ, your practice can reduce claim denials, improve collections, and maintain steady cash flow—all while cutting down on administrative overhead.
Ready to fix the leaks in your billing system? Schedule a demo with PracticeQ today.


